Subheadings:
– Lung pressures
– Compliance
– Resistance
– The act of breathing
Lung Pressures
What stops the lungs just collapsing down? What keeps them open?
The answer is a dynamic, constant tension of outward and inward forces, resulting in an equilibrium that keeps the lungs open. The main equation that explains how lungs remain open is:
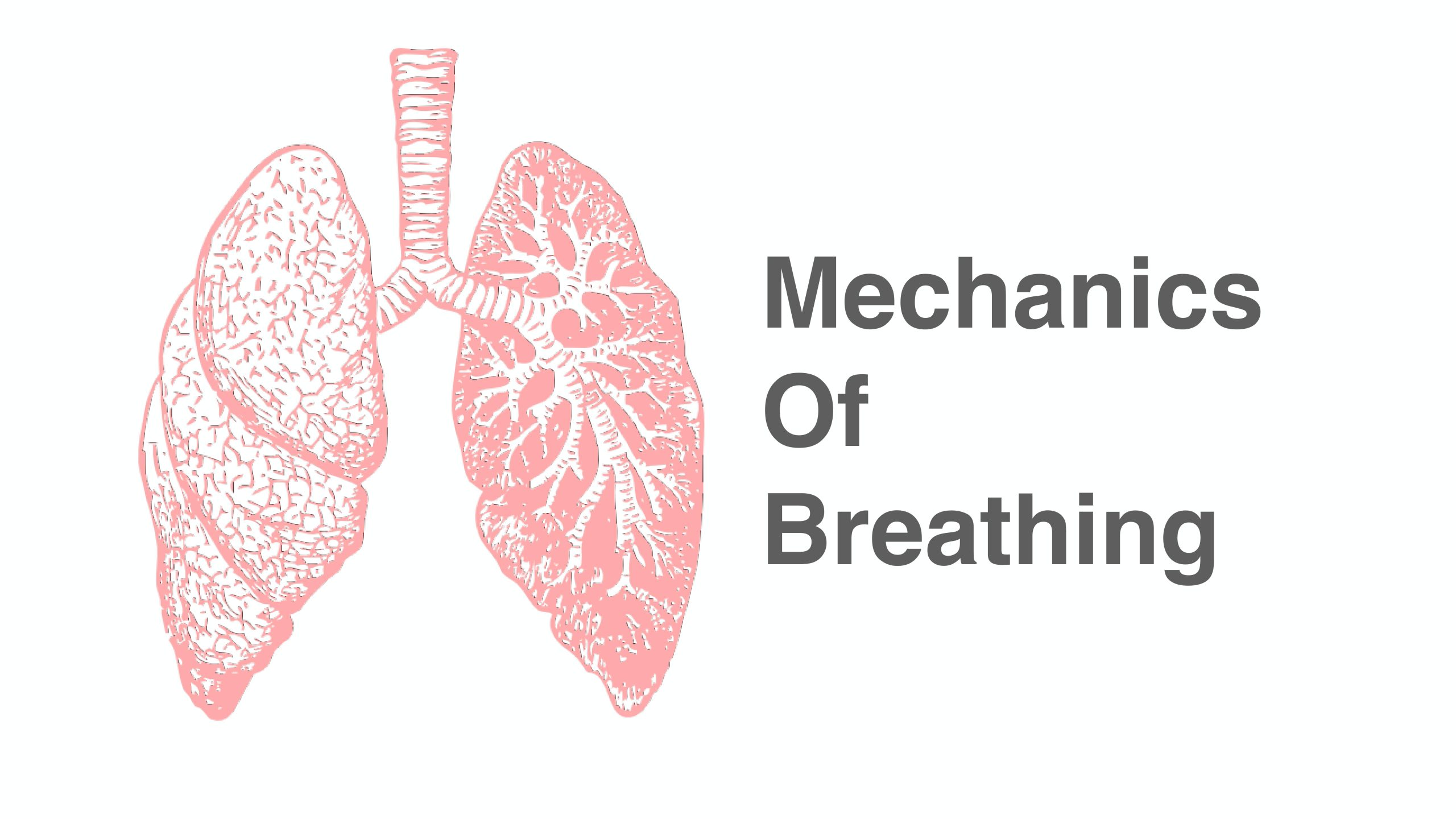
Transpleural pressure = intra-alveolar pressure – intrapleural pressure.
Let’s look at each of these components in a bit more detail.
Intrapleural pressure (IPP):
The thoracic cage and shape of the chest exerts an outward, upward pulling force against the lungs, whilst the lung tissues (particularly elastin and other connective tissues) exert an elastic recoil force, pulling inward against the chest wall.
These two opposing forces generate the intrapleural pressure; this is the negative pressure (caused by outward and inward forces of chest wall and lung elastic recoil, respectively) in the space between the visceral and parietal pleura of the lungs. The intrapleural pressure is normally around -4 mmHg in this space. The negative pressure pulls out the lung tissue, preventing collapse and maintaining alveolar and airway patency. Intrapleural pressure should remain negative at all times.
Intra-alveolar/intrapulmonary pressure (IAP):
Meanwhile, the intra-alveolar pressure (ie. inside the alveoli) when at rest is equal to the atmospheric pressure outside the body (0 mmHg). Inspiration will increase thoracic volume, cause a negative intra-alveolar pressure relative to the atmosphere (around -1 mmHg), which will draw air into the lungs. Expiration will shrink the thoracic volume, increasing intra-alveolar pressure (to around +1 mmHg), and forcing air out of the lungs into the atmosphere.
Transpulmonary pressure (TPP)
TPP illustrates the difference in pressure between the inside (intra-pulmonary pressure) and outside (intrapleural pressure, as the pleural space is the next space immediately outside) of the lungs, and is responsible for holding the lungs open.
Transpulmonary pressure (TPP) = intra-alveolar pressure (IAP) – intrapleural pressure (IPP)
IAP (0) – IPP (-4) = TPP (+4 mmHg)
The transpulmonary pressure always remains positive, which keeps the lungs inflated.
In a pneumothorax, there is a breach in the visceral pleura, causing an equalisation between the intra-alveolar and intra-pleural pressures. Both pressures then equal atmospheric pressure (0 mmHg), which causes the lung to collapse, as positive transplural pressure is lost, and there is no negative pressure in the pleural space to help keep the lungs pulled open. In this instance: IAP (0) – IPP (0) = TPP (0)
Compliance
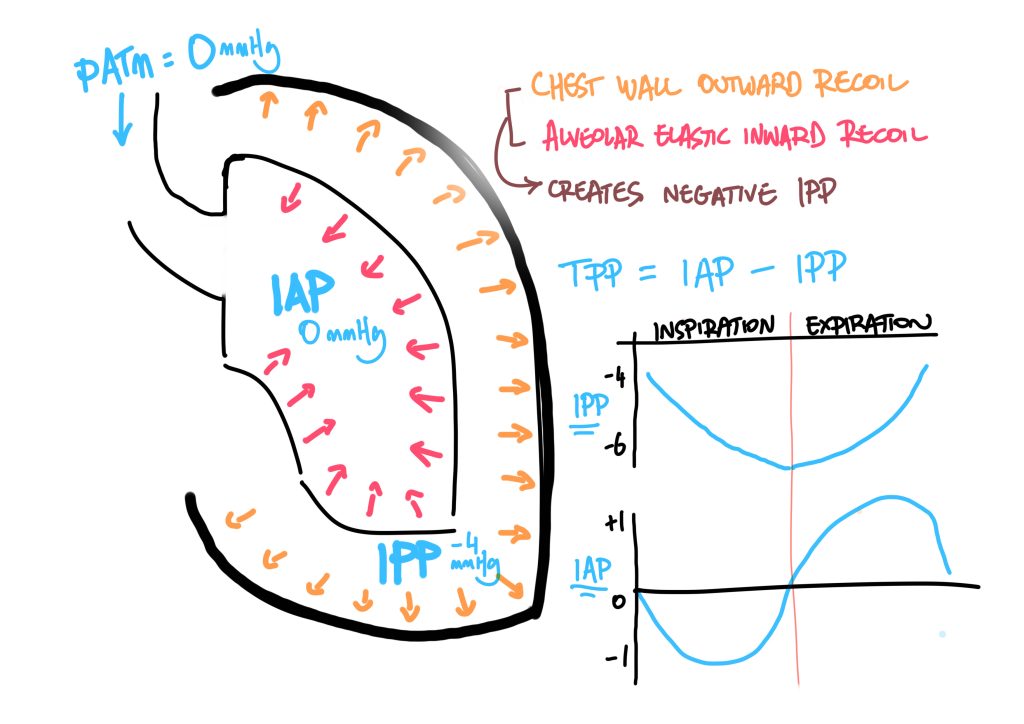
Compliance is defined as: the change in lung volume per unit of pressure.
In simple terms, this describes the amount of pressure (how much inspiratory force) is required to stretch the lung tissues, and in turn increase the space in the lungs to draw in air.
The volume of air inspired depends greatly on the degree of compliance. It will take much less pressure to generate a tidal volume of 500ml in healthy lungs (with normal tidal volume being about 7ml/kg), versus in ARDS, which will require much higher pressures to overcome the reduced compliance from inflammation and oedema.
Respiratory compliance = chest wall compliance + lung compliance.
Chest wall compliance factors:
- Chest wall shape
- Muscle tone
Factors affecting lung compliance:
- Elastic recoil
- Surface tension
Here, I will mainly focus on lung compliance.
Lung compliance follows a sigmoid curve; the initial flat area illustrates that it is harder to expand compressed alveoli than to expand partially opened ones. The steep incline shows that a much smaller amount of pressure is required for a much greater change in volume. The curve then flattens off again, because at higher volumes, greater pressures are required for ever smaller increases in volume; diminishing returns. Therefore, FRC (end of tidal expiration) , which sits in the middle of the lung compliance curve, is the point at which lungs are most compliant.
The two factors that affect lung compliance are:
- Elastic recoil in the lung tissue, which exerts an elastic, collapsing force on the alveoli, and is caused by elastin, collagen, and microfibrils within the parenchyma. Compliance can be increased by less elastin (such as in ageing and emphysema, where elastin is lost), or reduced by stiffer lungs (eg fibrosis, where tissue scarring makes lung tissue harder to expand).
- Surface tension is caused by the forces of attraction between water molecules within alveoli, which line the inner layer of alveoli and exert a collapsing, recoiling force. This is why multiple small water droplets on a surface tend to coalesce into a single larger droplet. Transpulmonary pressure is a force that helps to resist the total collapse of alveoli due to surface tension.
Problems caused by surface tension include:
- ↓alveolar radius (due to the inward, collapsing force) and ↓ compliance, requiring a higher transmural pressure to inflate the lungs.
- smaller alveoli will collapse into larger alveoli. This is because greater trans pulmonary pressures are required to open smaller alveoli versus larger alveoli. See point number 1; a smaller radius alveolus has lower compliance. Because transpulmoanry pressure is uniform through the lung, the smaller alveolus will collapse into its larger neighbour.
- transudate; the inward forces of surface tension attract more fluid into alveolar spaces, exacerbating poor compliance.
The problems with surface tension are counteracted by surfactant.
Surfactant
Surfactant is a substance, produced by type II pneumocystes in the alveoli, which contains phospholipids that repel each other outward. This, in turn, opposes the inward, collapsing forces of surface tension caused by water molecules, and increases alveolar compliance by resisting tendency to collapse inward.
Surfactant reduces surface tension in a non-linear manner; when compressed, the repelling forces are greater, and surface tension reduces even more. This is why surfactant stops smaller alveoli collapsing into larger ones.
Laplace’s law: Transmural Pressure = 2T/r
So, according to Laplace’s law, an alveolus with a smaller radius than its larger neighbour would have a higher transmural pressure and collapse into the larger one. Surfactant prevents this.
Factors affecting respiratory compliance (global compliance including lung and chest wall)
Increased compliance:
- Age (↓ elastin)
- Emphysema (↓ alveolar tissue = ↓ elastin)
- ↓ muscle tone eg neuromuscular disease (↓ ability to inflate lungs)
Decreased compliance:
- Alterations in lung volume and consolidation
◦ Pneumonia
◦ Pulmonary fluid
◦ ARDS
◦ Pneumonectomy - Increased surface tension
◦ Reduced surfactant - Reduced lung tissue compliance:
◦ Fibrosis - Decreased chest wall compliance
◦ Pregnancy/obesity
◦ Chest wall deformity/rigidity/burns - Poor posture
Resistance
Resistance is the energy lost in a flow of gas, due to friction or inertia. Higher degrees of resistance will impede gas flow more.
This is relevant to respiratory physiology where there can be varying degrees of airway resistance, and different types of gas flow (laminar versus turbulent). Airway resistance reduces further along the respiratory tree, with higher degrees of turbulent flow in the upper airways, and laminar flow further down in the respiratory zone. This is largely due to the higher velocities and branching airways in the upper zones then giving way to a greater surface area and, consequently, lower gas flow velocities.
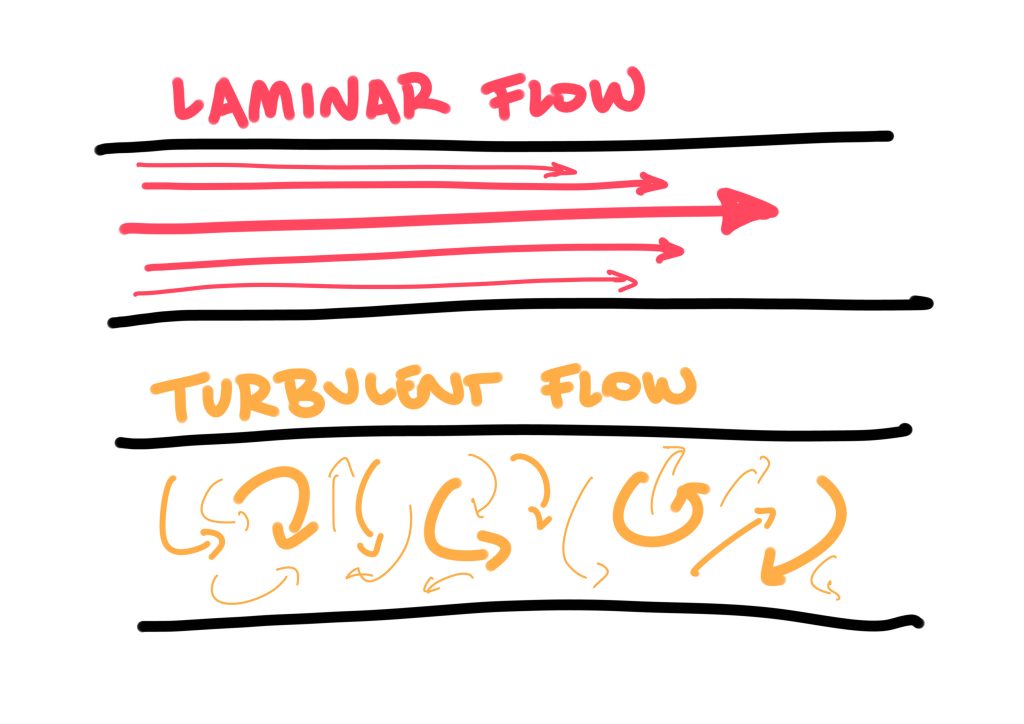
Laminar flow describes the flow of gases in a smooth, linear, parallel manner along a tube. Turbulent flow does not flow smoothly, but instead the direction, velocity and pressures are dispersed in a chaotic, random manner. This means that turbulent flows require greater pressures to maintain a gas flow, which in turn worsens turbulent flow and airway resistance. This is characteristic in bronchospasm, such as an asthma attack, where airway resistance and turbulent flow increase (causing wheeze) and, in turn, worsen the work of breathing required to ventilate.
An important concept is that there is a disproportionate decrease in flow rates, relative to a decrease in the diameter through which gas flows. This is captured in the Hagan-Poiseuille equation, where resistance to gas flow is proportional to r4 (r is the radius). This means that for each incremental reduction in the radius of a tube/airway, there is a reduction in gas flow to the power of 4. Therefore, small reductions in airway radius can have a large impact on the resistance to flow. This is true for any tube, including cannulas, chest drains etc.
This concept is important in clinical situations such as the following:
- Luminal obstruction such as bronchospasm and bronchoconstruction
- Intra-luminal obstruction such as mucous plugging or foreign body
- Any extra-luminal compression of airways eg tumours, haemorrhage, pleural effusion
This is why any incremental obstruction of a child’s airway can be precipitous, due to already having a small diameter and, thus, limited airflow. Any further narrowing of an already small airway, no matter how little, can have disproportionate consequences on air flow and ventilation.
The act of breathing
The act of respiration exerts additional pressure differences, enlarging and shrinking the lungs’ volume to breathe in and out. This pressure difference is generated as follows:
Inspiration: at rest, the diaphragm contracts, flattening downward and enlarging the thoracic cavity. If bigger breaths are needed, accessory muscles of the external intercostals, sternocleidomastoid and scalenes can increase intrathoracic, and consequently lung, volume.
On inspiration, intrapleural pressure decreases from -5 to -8 mmHg —> this exceeds the elastic recoil of lung tissue —> leads to lung expansion —> producing sub-atmospheric pressures within the alveoli —> air is drawn into lungs.
At rest, expiration is passive, with relaxation of the diaphragm generating a positive pressure within the lungs, returning the lung volume to FRC and expiring air out. If greater expired volumes are required, the abdominal muscles and internal intercostals are engaged as accessory muscles, squeezing the intrathoracic volume and consequently forcing more air out.
During expiration, the vocal cords slightly adduct, to maintain a physiologic positive end expiratory pressure (PEEP) of 3-4 mmHg, stenting alveoli open and preventing their collapse and atelectasis.
So, on reflection, what do we have to overcome to breathe in and ventilate?
- Any resistance caused by characteristics of the thorax and chest wall
- Elastic recoil of lungs
- Surface tension of alveoli
- Resistance of airflow
- Pathological components: anything that decreases compliance