Brief note:
I spent last year working with anaesthetic and critical care colleagues as part of my Emergency Medicine training. During this time, I gained a new appreciation for the application of physiology to clinical practice, and the usefulness of first-principles learning, for example, in altering ventilation settings in critically unwell patients. One particular anaesthetic consultant I worked with was able to explain virtually everything he did through the lens of physiology, and delivered hours of one-to-one, in-depth bedside teaching, whilst helping me learn the clinical practice of anaesthetics. His approach to teaching, his curiosity about the craft of his speciality, and his ground-up understanding of the underpinnings of his practice left a lasting impression on me.
Protocols and guidelines often supplant this kind of deep knowledge, but I’m more convinced that an understanding of physiology and basic sciences is required to move beyond technician toward mastery in clinical practice. This is especially true at the fringes of practice, where guidelines and protocols fail to encompass the grey areas of reality. To this end, I am making an effort to reinforce the more fundamental aspects of physiology. The purpose of these posts is to help me better synthesize and organize this knowledge for myself, and are a work in progress. Thankfully, as an EM trainee I’ve taken the executive decision to leave many of the equations and convoluted graphs to my anaesthetic colleagues.
Subheadings:
– The air we breathe
– Basic lung anatomy
The air we breathe:
The pressure of atmospheric air that we exist in is around 101 kPa, which is convenient for remembering its constituent gases as percentages (eg oxygen partial pressure is around 21 kPa, or around 21%). As we ascend into higher altitudes, the atmospheric pressure drops, but the fraction of oxygen remains around 21% (just that there is less O2 concentration).
This is a key concept; the proportion (%) of a gas can remain the same, whilst the partial pressure (kPa), or number of gas molecules within a given area, can differ.
For example, the atmospheric pressure at Everest is around a third of that at sea level, approximately 30 kPa (vs 101 kPa). This means that, although the fraction/percentage of oxygen is unchanged (around 21%), the concentration (or partial pressure) of oxygen is markedly reduced. In other words, there are less oxygen particles per unit area at a lower atmospheric pressure.
Conversely, higher atmospheric pressures can be found in hyperbaric chambers and deep sea diving (due to the gravitational pressure of water and, thus, gases). Saturation divers at 600 meters will be at an atmospheric pressure of around 6000 kPa (60 times that of sea level), and will only need around 2% O2 (rather than 21%) due to the increased partial pressure of oxygen; any more oxygen would risk significant oxygen toxicity effects.
- P = Partial pressure (kPa) = the actual concentration of a gas (eg PO2 = partial pressure of oxygen)
- F = Fraction = the proportion of a gas (eg FiO2 = fraction of inspired O2)
So what is in ‘air’?
Air is primarily a mixture of 3 gases (and some water vapor):
– Nitrogen (78 kPa / 78%)
– Oxygen (21 kPa / 21%)
– Carbon dioxide (0.03 kPa)
The approximation of 21 kPa PO2 (an absolute partial pressure) to 21% FiO2 (a relative proportion) for oxygen is not completely the same, since atmospheric air is 101 kPa (versus 100%). But regardless of altitude on earth, the relative proportions of each gas remains largely unchanged (eg 21% FiO2 at both sea level and top of Everest). The absolute partial pressure (PO2), however, is around a third at the summit of Everest vs sea level.
Function of the respiratory system
Fundamentally, respiratory physiology aims to facilitate gas exchange on a cellular level; the delivery of O2 and removal of CO2.
In addition, the respiratory system helps to maintain a homeostatic pH, some endocrine functions (eg angiotensin-converting enzyme), and vocalisation. But these are a moot point without gas exchange, first and foremost.
The goal is to get oxygen from outside, down to the cellular level for energy (ATP) production, and carbon dioxide from the cellular level, out to the external environment; all to maintain cellular respiration.
Basic lung anatomy
The right lung has 3 lobes (with a horizontal and oblique fissure) whilst the left has two lobes (with one horizontal fissure).
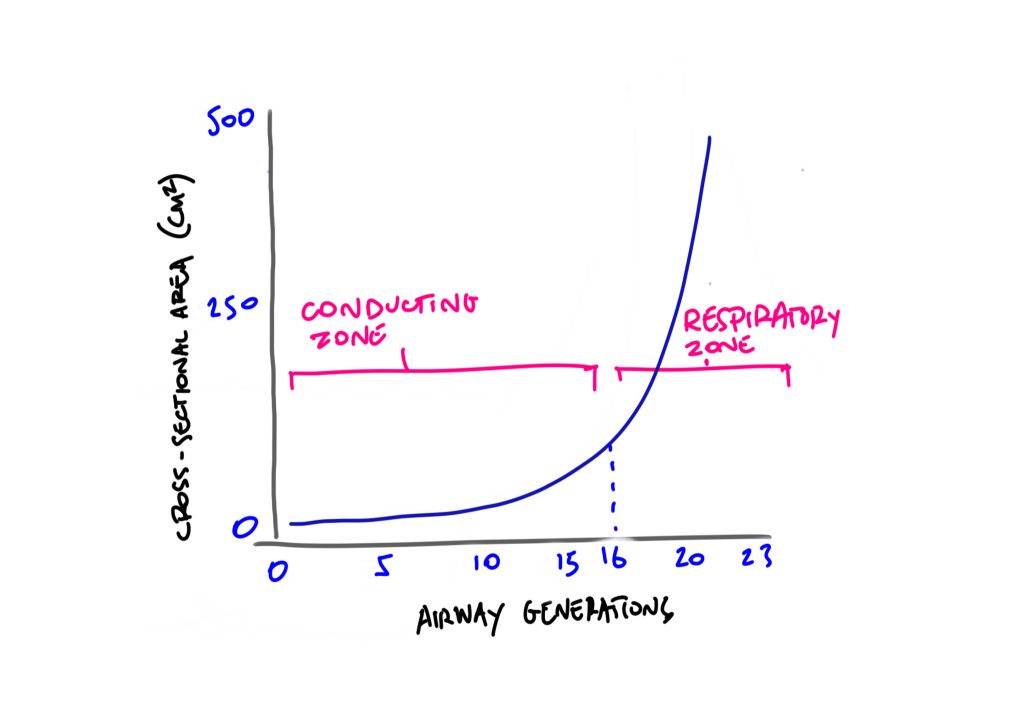
To keep things simple, the trachea bifurcates at the carina to the right and left main bronchi. These divide into lobar bronchi, then segmental bronchi, subsegmental bronchi, bronchioles, terminal bronchioles, respiratory bronchioles, alveolar ducts, and finally alveolar sacs. Each of these sequential branchings along the respiratory system are known as ‘airway generations’, and each generation contains roughly double the number of airways as the previous. If being pedantic, there are 23 airway generations in total (there are multiple generations for, eg respiratory bronchioles).
The lungs can be conceptually divided into the non-respiratory (the first 16 generations, which conduct the gases) and respiratory zones (which actually take part in gas exchange).
- The conducting (non-respiratory) zone consists of the trachea down to the terminal bronchioles (16th airway generation). This area makes up around 150ml, and is termed anatomical dead space, as no gas exchange takes place here.
- The respiratory zone encompasses the respiratory bronchioles and alveoli, and is approximately 3L in the average healthy adult.
Note: The right bronchus has a higher incidence of foreign body inhalation due to its wider shape and more vertical course.
This top to bottom system is conceptually termed the ‘respiratory tree’ (think of an upside down tree with the trachea as the trunk). The cross-sectional area increases exponentially from the respiratory bronchioles to the alveolar sacs, to increase surface area for gas exchange. On average, around 300 million alveoli offer up around 70 meters squared of gas exchange area.
The alveoli themselves are lined with pneumocyte cells.
- Type 1 pneumocytes are thin, specialized epithelial cells that make up around 90% of the lining; their thin permeable nature permit gas exchange between the capillaries and alveoli.
- Type 2 pneumocytes produce and metabolise pulmonary surfactant.
- Finally, macrophages are also present that engulf inspired particles such as bacteria.
Surface landmarks
- Trachea starts at C6 (border of cricoid cartilage)
- Trachea bifurcates into right and left main bronchi at T4/5 level at the carina (approx 20-25cm from lips, depending on sex and height)